Quantifying Fall Risk: How AM-PAC Scores Drive Better Patient Outcomes
The Activity Measure for Post-Acute Care (AM-PAC) is an outcome measure that scores mobility, daily activity, and applied cognitive functions to help clinicians assess fall risk, reduce falls, and provide better care. AM-PAC is a critical piece of fall prevention protocols, especially as our population ages.
February 4, 2025
7 min. read

The Activity Measure for Post-Acute Care (AM-PAC) is a common measure used by healthcare organizations that provides insight into mobility limitations, a key risk factor of falls, and can be applied across settings, from acute care to outpatient rehabilitation and continue when the patient is in their home.
How Are AM-PAC Scores Used?
The AM-PAC can be used in combination with other tools to improve fall risk assessment, reduce the number of falls, and provide better patient care, ultimately providing more complete information about a patient's risk of falling. These can include other widely-used assessment metrics like the STEADI (Stopping Elderly Accidents, Deaths, and Injuries) toolkit. Developed by the CDC, STEADI offers a range of free tools designed to help clinicians screen, assess, and intervene in fall risk, providing a structured framework to support better patient outcomes.
Together, these tools can help providers determine exercise guidelines (such as strength-based exercises), identification of hazards around the home (loose rugs or lack of bathroom grab bars), or dual-task training (in which a patient actively practices engaging in two or more things simultaneously to reduce the risk of falling during daily activities—such as walking while talking on the phone).
Why Do AM-PAC Scores Matter?
It's especially critical to understand these outcomes measures as the entire ‘Baby Boomer’ generation becomes Medicare-eligible by 2030. With this dramatic increase in Medicare beneficiaries comes a global public health concern often associated with aging—falls and fall-related injuries.
Falls and fall-related injuries are preventable, however, and healthcare organizations and clinics need additional resources in order to keep up with the demands. These cascading challenges are reshaping how healthcare organizations approach patient safety and care delivery, but to scale the level of care this generation needs, expanding access to proactive, preventative care will be essential. Knowing how to use and interpret outcomes measures such as AM-PAC and/or STEADI will be crucial to providing this care.
Motion Capture and Fall Prevention
There are also advanced technological tools like motion capture that can assist in fall risk assessment in addition to more traditional tools like AM-PAC or STEADI. For example, Medbridge Pathways provides an AI-assisted motion capture assessment to help the physical therapist analyze the patient’s movements. The clinician can use this additional piece of data, along with tools like AM-PAC, or the STEADI tool, to determine if the patient is at higher risk of falling and develop a personalized fall management plan within Pathways.
Better prevention will be key to reducing falls and fall-related injuries, and ultimately helping stabilize our overburdened healthcare system.
The Growing Need for Fall Prevention Programs
Among older adults seeking physical therapy, 44 percent are at an increased risk of falling as they progress through their treatment plan.1 However, only 23 percent of older adults classified as moderate fall risk receive rehabilitation services, and only 13 percent have their fall risk addressed during physical therapy.2 These care gaps are often caused by limited provider capacity and geographic barriers that can hinder access to care for many older adults at risk of falling. Without adequate fall risk prevention, many older adults have to risk falls to seek care in the first place!
Contrary to popular belief, falls are not a “normal” part of aging, and can be reduced with the right prevention strategies. Falls are, however, much more prevalent among older adults compared to other populations. One in four older adults in the United States will fall every year, and falls are the leading cause of injuries in this population, including hip fractures and traumatic brain injuries.3 This number rises among community-dwelling older adults, where approximately 33 percent of this population will fall at least once a year.4
These care gaps produce a significant risk to the patient, but are also extremely costly, which has downstream effects for the entire healthcare industry. It’s estimated that falls in older adults cost the U.S. healthcare system approximately $50 billion annually5—money and resources that could be much better spent on preventative measures that reduce falls in the first place. For example, one study found that effective physical therapy interventions can lead to an average net savings of $2,144 per episode of care.6
When it comes to falls, prevention is key. If you’re able to predict and prevent a fall, you’re able to be proactive about achieving your care goals—and that’s where AM-PAC comes in.
AM-PAC Score Chart PDF
Fill out the form to unlock your free PDF!

How to Apply AM-PAC Data to Fall Prevention
AM-PAC scoring data helps identify individuals with mobility limitations that often result in high risk of falling. The data can shape the fall prevention program from inception and serve as a guide to measure patient progression through the program.
Adopting digitally-driven exercise programs and self-managed fall prevention solutions, like those found in Pathways, can also significantly reduce fall rates—for example, one study showed a 23 to 42 percent reduction in fall rate from regular exercise (constituting 150 minutes per week of moderate-to-vigorous physical exercise, emphasizing strength training twice per week and balance training once per week).7 Digitally managed exercise programs also make exercise progression easy and tracking of patient adherence is often built it.
Another impactful strategy is incorporating remote therapeutic monitoring (RTM). RTM helps clinicians monitor patient progress and gather objective data outside the clinic, which is immensely valuable when determining a care plan. This can help in a variety of ways, such as illustrating readiness of discharge (or lack thereof), monitoring progress, and collecting data from the patient’s home environment. Many falls occur inside the patient’s home, so gaining insight into the patient’s home environment helps to provide more personalized care.
Combining AM-PAC scoring data with other data points such as exercise duration or adherence markers and RTM can provides a holistic, data-driven, fall prevention program.
What An Effective Fall Prevention Program Looks Like
Medbridge’s Fall Prevention Pathways program proactively engages patient populations with dynamic fall prevention programs that improve balance, boost confidence, and help reduce the risk of falls. These evidence-based, medical board-reviewed clinical programs are designed to engage patients and improve care at scale. They work well alongside assessments such as AM-PAC and/or STEADI.
First, patients are prompted to complete the Short Falls Efficacy Scale at baseline (or the first day of starting their program) and at the start of every week. This is used to assess the patientʼs progress with fear of falling over time. Patients are also asked to report if they have fallen in the past week at the start of each week. This covers topics like:
1. Getting dressed or undressed
2. Taking a bath or shower
3. Getting in or out of a chair
4. Going up or down stairs
5. Reaching for something above your head or on the ground
6. Walking up or down a slope
7. Going out to a social event
Then, Pathways utilizes two different functional assessments that are assessed weekly:
30 Second Sit-to-Stand
Clinically validated
Easy instructions to follow
Built-in safety
Clinically validated
Excellent clinical information gathered
Relatively safe, calls for keeping support within arm’s reach
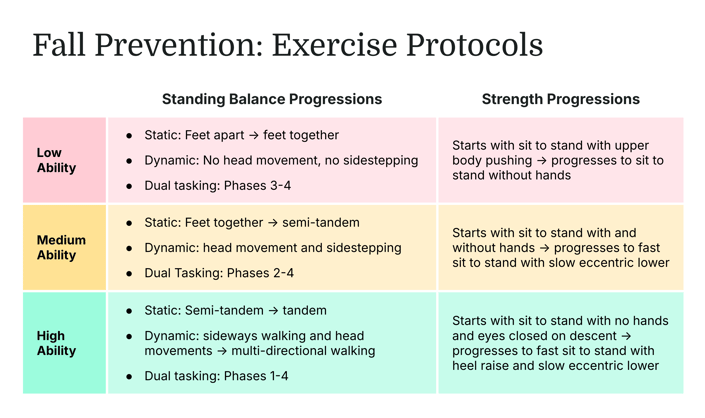
Next, Pathways begins a phased progression exercise program that is tailored to each patients’ unique needs. For example, their program could look something like this:
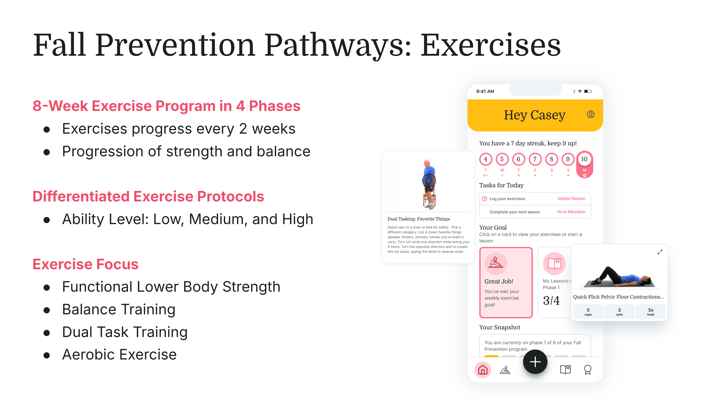
Because they are prescribed by a clinician, each Pathways program can be adjusted to fit the patient’s current ability.
Each pathway is supplemented with holistic education, providing interactive video education that engages learners with the four Ms: movement, management, modifications, and mind.
In the end, you get a dynamic, effective fall prevention program personalized to each patient. To learn more about how Pathways can help you proactively engage your population with dynamic fall prevention programs that improve balance, boost confidence, and help reduce the risk of falls, request a demo.
References
- Vincenzo JL, Bergen G, Casey CM, Eckstrom E. Reframing Fall Prevention and Risk Management as a Chronic Condition Through the Lens of the Expanded Chronic Care Model: Will Integrating Clinical Care and Public Health Improve Outcomes? Gerontologist. 2024 Jun 1;64(6):gnae035. doi: 10.1093/geront/gnae035. PMID: 38666718; PMCID: PMC11149378.
- Gell NM, Patel KV. Rehabilitation Services Use of Older Adults According to Fall-Risk Screening Guidelines. J Am Geriatr Soc. 2019 Jan;67(1):100-107. doi: 10.1111/jgs.15625. Epub 2018 Oct 8. PMID: 30295320; PMCID: PMC6322948.
- Kakara, R., Bergen, G., Burns, E., & Stevens, M. (2023). Nonfatal and fatal falls among adults aged ≥65 years—United States, 2020–2021. MMWR Morbidity and Mortality Weekly Report, 72, 938–943. https://doi.org/10.15585/mmwr.mm7235a1
- AGS Journals, 2021
- CDC, 2018
- Value of PT Report, 2023
- Sherrington C, Fairhall N, Kwok W, Wallbank G, Tiedemann A, Michaleff ZA, Ng CACM, Bauman A. Evidence on physical activityand falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentarybehaviour. Int J Behav Nutr Phys Act. 2020 Nov 26;17(1):144. doi: 10.1186/s12966-020-01041-3. PMID: 33239019; PMCID:PMC7689963.





